Abstract
Introduction. Hematologic recovery is often not satisfactory in patients undergoing an allogeneic stem cell transplantation (HSCT). A significant proportion have been reported to have low peripheral blood counts, despite full donor chimerism. This condition can be related to several factors including: number of CD34+ cells infused , stem cell source, underlying disease, conditioning regimen, GvHD and viral infections. Recently transplant platforms have changed, including the use of haploidentical transplants and modified GvHD prophylaxis.
Aim of the study: to investigate factors associated with hematological recovery following an allogeneic HSCT in current transplant years.
Methods: We included 1311 patients, with hematological diseases, undergoing an allogeneic HSCT, between year 2000 and 2020, in two transplant center: Genova and Roma. The main diagnoses were acute leukemia (54%), lymphoproliferative disorders (13%) , myelodysplastic syndromes (9%) and myelofibrosis (9%). 1108 patients aged <60 years and 203 aged >60 years. Platelet counts were taken as a surrogate marker of hematologic recovery.
Results: We first ran a multiple regression analysis on factors influencing platelet counts between 50 and 100 days post-transplant. These factors were patients age >60 years, GvHD grade II-IV, non sibling donor and a diagnosis of myelofibrosis.
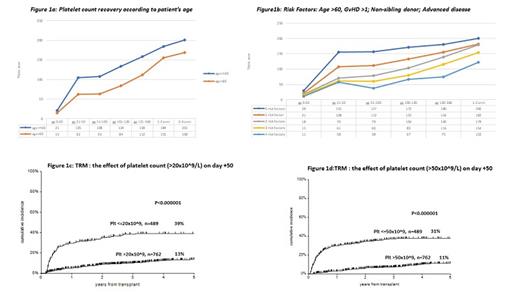
Platelet recovery at different time points, up to over 4 years post-transplant, is shown in Figure 1a in patients stratified according to an age cut off of 60 years. Patients younger than 60 years showed significantly improved platelet recovery , at each time point, when compared to patients over 60 years ; the difference persisted beyond 4 years. There was no difference in platelet recovery in patients aged 18-40 and 41-60. Donor age and year of transplant had no effect on platelet recovery. Figure 1b shows platelet recovery according to risk factors (age, GvHD, myelofibrosis, non sib donor).
Transplant related mortality (TRM). We then asked whether low platelet counts predicted TRM. Patients with a platelets count higher than 20 and 50x10^9 on days 50-100 post-HSCT, showed a reduced transplant related mortality (TRM) as compared to patients with a lower platelet count (13%vs 39%: p<0.000001; 11% vs31%, p<0.000001) (Figure 1 c,d).
Conclusions: Platelet recovery post-HSCT seems to be strongly influenced by patient's age, together with GvHD, a diagnosis of myelofibrosis and donor type. Slow recovery in older patients remains statistically significant beyond 4 years after HSCT. Hematologic recovery after HSCT has not improved over the past 2 decades. Low platelet counts are a strong risk factor for mortality after allogeneic HSCT. Clinical trials with TPO agonists post HSCT are warranted to assess whether hematologic recovery can be improved, and whether this will translate in reduced mortality.
Sica: Pfizer: Honoraria. Laurenti: AstraZeneca: Consultancy, Honoraria; AbbVie: Consultancy, Honoraria, Research Funding; Janssen: Consultancy, Honoraria; Roche: Honoraria, Research Funding; Gilead: Honoraria; BeiGene: Honoraria. Metafuni: Jazz: Other: Invited Clinical case presentation at meeting. Angelucci: Novartis: Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Celgene BSM: Honoraria, Other: DMC; Blue Bird Bio: Honoraria, Membership on an entity's Board of Directors or advisory committees; Menarini-Stemline: Honoraria, Membership on an entity's Board of Directors or advisory committees, Other: steering commitee, Speakers Bureau; Vertex Pharmaceuticals: Honoraria, Other: DMC; Crispr therapeutics: Honoraria, Other: DMC; Glaxo: Honoraria, Membership on an entity's Board of Directors or advisory committees; Gilead: Honoraria, Membership on an entity's Board of Directors or advisory committees.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal